Joint Replacement Surgeries: Also known as Arthroplasty is surgery to replace all or some of a joint. Your surgeon will replace worn-out or damaged bone and cartilage in your natural joint with a prosthetic implant. It usually takes at least a few months to recover after an arthroplasty. Your recovery time will depend on which joint needs a replacement.
Overview
What is arthroplasty?
Arthroplasty is a surgical procedure to replace some or all of a joint. Healthcare providers also call it joint replacement surgery or joint replacement. A surgeon will remove the worn-out or damaged parts of your natural joint and replace them with an artificial joint (a prosthesis) made of metal, plastic or ceramic.
Types of arthroplasties:
Any large joint can be replaced with an arthroplasty, including your:
- Hips.
- Knees.
- Shoulders.
- Ankles.
- Elbows.
- Wrists.
- Fingers.
- Toes.
Your surgeon will suggest either a total or a partial joint replacement:
- Total joint replacement (total arthroplasty): During a total joint replacement, your surgeon will replace all the parts of your joint with a prosthetic joint.
- Partial joint replacement (partial arthroplasty): A partial joint replacement is just what it sounds like. Your surgeon will replace only some parts of your joint. Some healthcare providers sometimes refer to this as joint resurfacing.
What does arthroplasty help treat?
A healthcare provider might recommend joint replacement surgery if you have severe symptoms that don’t get better after trying nonsurgical treatments like activity modifications, physical therapy or medications. Symptoms that can cause you to need an arthroplasty can include:
- Joint pain.
- Stiffness or decreased range of motion (how far you can move a joint).
- Limited mobility (difficulty physically moving because of your affected joint).
- Swelling.
- Instability.
Arthritis is the most common reason people need an arthroplasty. Most people who choose to have a joint replacement have osteoarthritis, but some people with rheumatoid arthritis may need one, too.
A healthcare provider might suggest an arthroplasty if you’ve experienced a bone fracture (broken bone) in your joint or if you have post-traumatic arthritis. Trauma that causes fractures or post-traumatic arthritis can include:
- Falls or other serious injuries.
- Car accidents.
- Sports injuries.
Procedure Details
How should I prepare for an arthroplasty?
Your healthcare provider or surgeon will help you get ready for surgery. You might need:
- A physical exam to make sure you’re healthy enough for surgery.
- Blood tests.
- An electrocardiogram (EKG) to check your heart health.
- A dental exam to reduce your risk of developing an infection after surgery.
- Imaging tests, including X-rays. You might also need magnetic resonance imaging (MRI) or a computed tomography (CT) scan.
Tell your provider and surgeon about any medications and over-the-counter (OTC) supplements you take. You may have to stop taking them before your surgery. Your surgeon will tell you when you should stop eating and drinking the day before your surgery. Most people need to avoid eating and drinking for eight hours before their surgery. Your surgeon will tell you which medications are safe to take with a sip of water the morning of your surgery.
What happens during an arthroplasty?
The day of your surgery you’ll receive anesthesia to numb your body and make sure you don’t feel any pain. An anesthesiologist will give you either general anesthesia to put you to sleep during your surgery or regional anesthesia to numb the area around your joint that needs replacing. They may give you other medications to make you sleep if you need regional anesthesia.
-
During a joint replacement, your surgeon will:
- Remove damaged cartilage and bone.
- Insert the prosthetic joint.
- Insert other prosthetic parts to recreate your natural tissue. They might use spacers to mimic natural cartilage, for example.
- Reshape the bones around your joint to fit the new prosthetic (if they need to).
Robotic-assisted joint replacement:
Some types of arthroplasties can be done as robotic-assisted joint replacements. This doesn’t mean a robotic surgeon does the procedure automatically — it’s a special technique to help your surgeon. During a robotic-assisted arthroplasty, your surgeon will use a special computer that guides their surgical tools during the operation. Studies have found that robotic-assisted joint replacements can be more accurate and insert prosthetic implants more securely.
It’s most common for surgeons to use robotic assistance to replace bigger joints like hips and knees.
How long does an arthroplasty take?
Arthroplasties usually take a few hours from start to finish. It depends on which of your joints needs a replacement, and if you’re getting a total or partial joint replacement.
What happens after an arthroplasty?
After surgery, you’ll be moved to a recovery room. Your surgery team will keep an eye on you for a few hours to make sure you wake up from the anesthesia without complications. They’ll also monitor your vital signs and pain level. Some people who have joint replacement surgery go home the same day. You might need to stay in the hospital overnight or for a few days. Your surgeon will tell you when it’s safe for you to go home.
Risks vs Benefits:
What are the pros and cons of joint replacement?
For most people, the benefits of a joint replacement far outweigh the risks. An arthroplasty is a major surgery, and that means there’s always a chance you experience complications. However, many people who have a joint replacement experience a big, noticeable improvement in their daily routines — especially if they’ve been living in pain for a long time.
Certain health conditions can make recovery from an arthroplasty more difficult. Talk to your surgeon about your health history. Tell them if you have:
- Hemophilia.
- Diabetes.
- Other autoimmune diseases (like lupus).
Talk to your healthcare provider or surgeon about the risks of a joint replacement. They’ll help you decide if arthroplasty is right for you.
Benefits of arthroplasty
Arthroplasty is a safe, effective procedure that helps people regain their mobility and relieves long-term pain. Most people who have a joint replacement have an increased quality of life because they can move better with less pain.
Arthroplasty complications
Some people who have joint replacement surgery still experience pain and other symptoms in their affected joint. Rare complications include:
- Blood clots.
- Infection inside your joint or at your surgery site.
- Nerve damage (including foot drop).
- Blood vessel damage.
- Problems with the prosthetic implant, including the device wearing down too soon or loosening.
- Scar tissue inside your joint.
- Reduced range of motion and stiffness.
Your surgeon will tell you what you can expect after your surgery and how you can reduce your chances of experiencing complications. It’s important to follow your surgeon’s and physical therapist’s recovery instructions and to avoid limping after your surgery. Moving unusually or unnaturally can cause tendinitis or bursitis.
How long does a joint replacement last?
A joint replacement usually lasts a long time. Many people who have a joint replacement live with it for the rest of their lives. It’s rare, but some people need additional surgeries on that same joint in the future. Your surgeon will tell you what to expect.
What is the recovery time after an arthroplasty?
It depends on which joint was replaced. It usually takes at least a few months to recover after an arthroplasty. Everyone’s body responds differently to joint replacement surgery.
Your recovery time will depend on several factors, including:
- Which joint was replaced.
- If you had a total or partial arthroplasty.
- Your activity level before surgery.
- Your age.
- Other health conditions you have.
Your surgeon will give you a customized recovery plan, but in general, you should:
- Ice your joint: Icing your joint a few times a day for 20 minutes at a time will help relieve pain and swelling.
- Elevate your joint: Keep your joint above the level of your heart as often as possible. You can prop it up on cushions or pillows while lying down.
- Keep your incision clean and covered: Follow your surgeon’s incision care instructions carefully to prevent infections. Ask your surgeon when you should change the dressing on your incision site and when it’s safe to take a shower or bathe.
- Home exercises: Your surgeon will give you exercises to do as soon as possible after your surgery. They’ll show you how to perform movements and exercises to strengthen the muscles around your joint and prevent stiffness. Do your exercises as often as your surgeon instructs. They’ll help your recovery and make sure your joint regains its function.
- Physical therapy: You’ll work with a physical therapist for up to a few months after your surgery. They’ll help you start moving safely. People who have knee replacements should start moving their joint as soon as possible after surgery. Your surgeon will give you instructions about how to move your joint safely before you go home after your arthroplasty.
- Avoid movements that may cause dislocations: All newly replaced joints have a temporarily increased dislocation risk (especially hips and shoulders). You may need to avoid certain body positions or movements that can cause dislocations for up to six months after your arthroplasty. Your surgeon or physical therapist will tell you what’s safe and which movements to avoid while you recover.
Pain management after arthroplasty
After surgery, you’ll feel pain, especially in the first few weeks of your recovery. You’ll feel pain from the surgery itself and pain as your body begins to heal.
Your surgeon will suggest a combination of prescription pain medication, over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) — if it’s safe for you to take them — and acetaminophen to relieve your pain. Your surgeon will tell you how much of each kind of medication you can take each day or in a certain amount of time.
Talk to your surgeon if you feel like you’re experiencing too much pain or if you’re worried about any complications from taking pain medication.
What can I do to help my recovery at home?
Ask your surgeon or physical therapist for tips to move through your home safely after your surgery. They can show you how to safely:
- Walk and move.
- Sit down and stand up.
- Go to the bathroom.
- Bathe or shower.
- Get dressed.
- Use stairs.
When can I go back to work or school after an arthroplasty?
How long you’ll need to miss work or school depends on how much stress your job or other activities put on your affected joint. Most people need to rest at home for a few weeks. Your surgeon will tell you when it’s safe to return to work or school.
When should I call my healthcare provider?
Call your surgeon or healthcare provider right away if you experience any of the following symptoms:
- Chest pain.
- Shortness of breath (dyspnea).
- Fever higher than 101 degrees Fahrenheit (39 degrees Celsius).
- Bleeding.
- Signs of infection at your surgery site, including leaking, swelling, discoloration, odor or a feeling of warmth.
- New or worsening pain in your calf, ankle or foot.
- Severe pain that doesn’t get better after you take pain medication.
A note from Dr. Om Prakash Agrawal:
Choosing to have an arthroplasty (joint replacement surgery) is a big decision. Talk to your healthcare provider and surgeon before you decide to have a joint replacement. Most people who have an arthroplasty experience a noticeable improvement in their quality of life. Joint replacements can relieve symptoms like pain, stiffness and difficulty moving.
After your surgery, you’ll need time to strengthen your muscles and heal your body. Take your recovery slow and don’t rush yourself. Talk to your surgeon or physical therapist about your movement goals and which activities you’d like to participate in after your joint replacement.
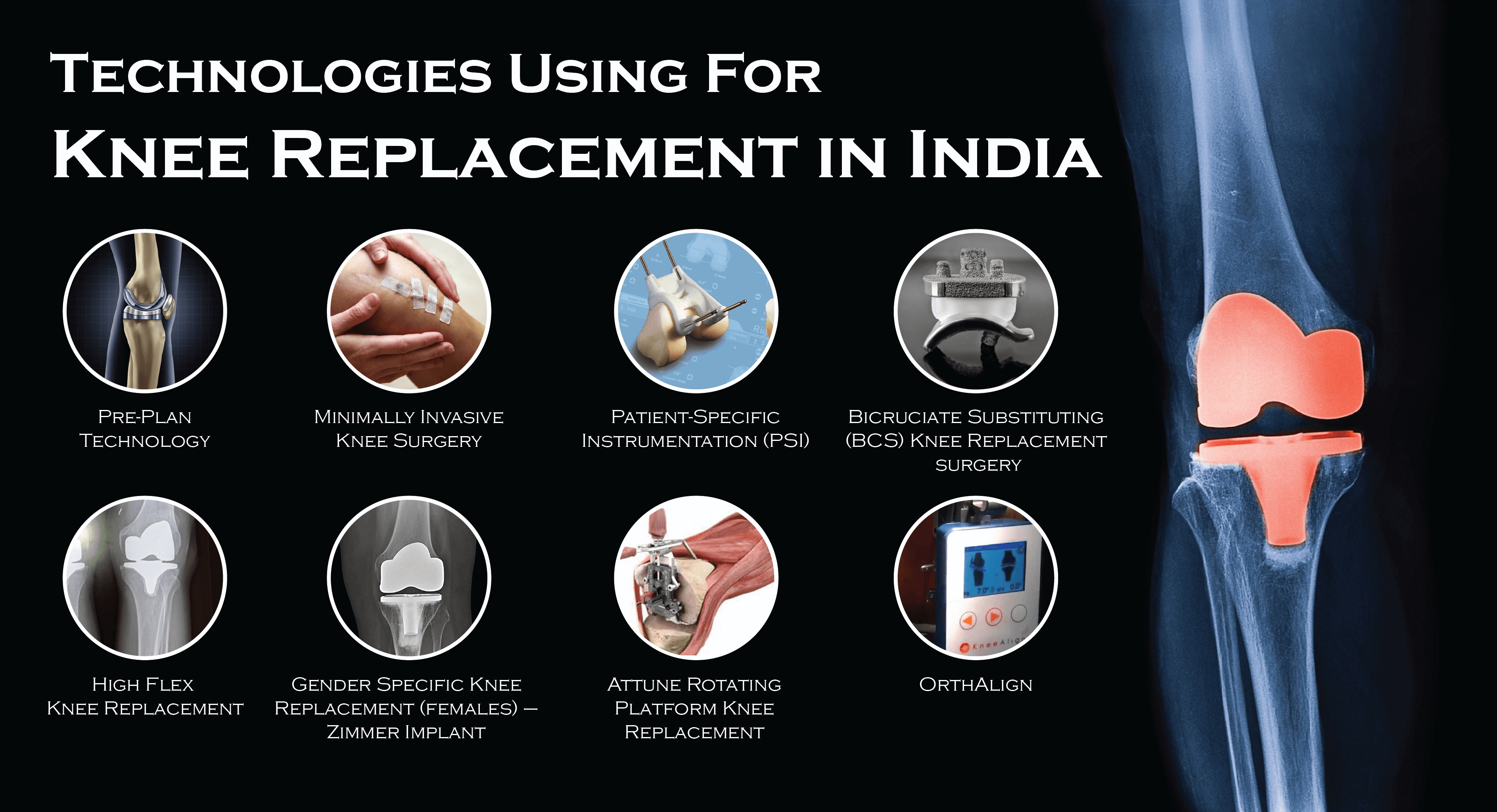
Knee Replacement Surgery:
Knee replacement surgery (knee arthroplasty) is surgery to replace all or some of your knee joint. Your surgeon will replace damaged cartilage and bone with a prosthetic joint. It can take up to a year to recover fully after a knee replacement, but you’ll be able to resume some of your usual activities gradually as you heal.
What is knee replacement surgery?
A knee replacement is surgery to replace all or some of your knee joint. It’s a type of procedure called an arthroplasty (joint replacement). A surgeon will remove damaged parts of your natural knee joint and replace them with an artificial joint (a prosthesis) made of metal and plastic.
Types of knee replacement:
Your surgeon will recommend either a total or partial knee replacement:
- Total knee replacement: Total knee replacement is the most common type of knee replacement. Your surgeon will replace all three areas of your knee joint — the inside (medial), outside (lateral) and under your kneecap (patellofemoral).
- Partial knee replacement: A partial knee replacement is just what it sounds like. Your surgeon will only replace some areas of your knee joint — usually if only one or two areas are damaged. Partial knee replacements are more common in younger adults who’ve experienced an injury or trauma.
What conditions are treated with a knee replacement?
A healthcare provider might recommend knee replacement if you have severe symptoms that don’t get better after trying nonsurgical treatments, including:
- Joint pain
- Stiffness
- Limited mobility (trouble moving your knee)
- Swelling
Arthritis is the most common condition that causes people to need knee replacement surgery. Most people who choose to have a knee replacement have osteoarthritis, but some people with rheumatoid arthritis may need one, too.
It’s rare, but a healthcare provider might suggest knee replacement if you’ve experienced a bone fracture in your knee that causes post-traumatic arthritis after you’ve experienced a:
- Car accident
- Fall
- Sports injury
How common is knee replacement surgery?
Knee replacements are one of the most common types of arthroplasties. Surgeons in India perform more than 10, 00,000 knee replacements each year.
How should I prepare for a knee replacement?
Your healthcare provider and surgeon will tell you what you need to do to get ready for surgery. In general, you’ll need:
- A physical exam to make sure you’re healthy enough for surgery.
- Blood tests.
- An electrocardiogram to check your heart health.
- A dental exam to reduce your risk of developing an infection after surgery.
- Imaging tests, including a knee X-ray. You might also need magnetic resonance imaging (MRI) or a computed tomography (CT) scan.
Tell your doctor and surgeon about any medications and over-the-counter supplements you take. You may have to stop taking some medications or supplements before your surgery.
Your surgeon will tell you when you should stop eating and drinking the day before your surgery. Most people need to avoid eating and drinking 12 hours before their surgery.
What happens during a knee replacement?
On the day of your surgery, you’ll receive anesthesia to numb your body and make sure you don’t feel any pain. An anesthesiologist will give you either general anesthesia to put you to sleep during your surgery or a regional anesthesia to numb you from the waist down.
During a knee replacement, your surgeon will:
- Remove damaged cartilage and bone.
- Insert the prosthetic knee joint.
- Insert a plastic spacer that recreates the smooth cushion of your cartilage that was damaged or removed.
- Reshape your patella (kneecap) to fit the new prosthetic knee joint (if needed).
How long does a knee replacement take?
Knee replacements usually take an hour or two.
What happens after a knee replacement?
After surgery, you’ll be moved to a recovery room. Your surgery team will keep an eye on you for a few hours to make sure you wake up from the anesthesia without complications. They’ll also monitor your vital signs and pain level. Some people who have knee replacement surgery go home the same day. You might need to stay in the hospital overnight. Your surgeon will tell you when it’s safe for you to go home.
What are the benefits of knee replacement surgery?
Knee arthroplasty is a safe, effective procedure that helps people regain their mobility and relieves long-term pain. Most people who have a knee replacement have reduced pain, increased ability to move and use their knee, and improved quality of life.
How does a knee replacement last?
A knee replacement usually lasts a long time. In fact, more than 90% of people who have knee replacement surgery have improved function in their knee for 10 to 15 years.
What are potential complications of a knee replacement?
Some people who have knee replacement surgery still experience pain and other symptoms in their knee. Rare complications include:
- Blood clots.
- Infection inside of your knee or at your surgery site.
- Nerve issues.
- Blood vessel issues.
- Problems with the prosthetic implant, including the device wearing down too soon or loosening.
- Scar tissue inside of your knee.
- Reduced range of motion (how far you can move your knee) and stiffness.
Certain health conditions can make recovery from a knee replacement more difficult. Talk to your surgeon about your health history. Tell them if you have:
- Hemophilia.
- Diabetes.
- Other autoimmune disorders (like lupus).
Your surgeon will let you know what to expect after your surgery and how you can reduce your chances of experiencing complications.
How long does it take to recover from a knee replacement?
It usually takes around a year to recover fully after a knee replacement. But you should be able to resume most of your usual activities six weeks after surgery.
Your recovery time will depend on several factors, including your:
- Activity level before surgery.
- Age.
- Other health conditions.
Your surgeon will give you a customized recovery plan, but in general, you should:
- Ice your knee: Icing your knee a few times a day for 20 minutes at a time will help relieve pain and swelling.
- Elevate your knee: Keep your knee above the level of your heart as often as possible. You can prop it up on cushions or pillows while lying down or rest it on a footstool if you’re sitting in a chair.
- Keep your incision clean and covered: Follow your surgeon’s incision care instructions carefully. Ask your surgeon when you should change the dressing on your incision site and when it’s safe to take a shower or bathe.
- Home exercises: Your surgeon will give you exercises to do as soon as possible after your surgery. They’ll show you how to perform movements and exercises to strengthen the muscles around your knee and prevent stiffness. Do your exercises as often as your surgeon instructs. They’ll help your recovery and make sure your joint regains its function.
- Physical therapy: You’ll work with a physical therapist for up to a few months after your surgery. They’ll help you start moving safely, including bending your knee and walking.
Pain management after knee replacement:
After surgery, you’ll feel pain, especially in the first few weeks of your recovery. You’ll feel pain from the surgery itself and pain as your body begins to heal.
Your surgeon will suggest a combination of prescription pain medication, over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) (if it’s safe for you to take them) and acetaminophen to relieve your pain. Your surgeon will tell you how much of each kind of medication you can take each day or in a certain amount of time.
Talk to your surgeon if you feel like you’re experiencing too much pain or if you’re worried about any complications from taking pain medication.
When can I go back to work or school after a knee replacement?
How long you’ll need to miss work or school depends on how much stress your job or other activities put on your knee. Most people need to rest at home for a few weeks after a knee replacement. Your surgeon will let you know when it’s safe to return to work or school.
What can I do to help my recovery after a knee replacement?
You’ll be able to walk with a cane or a walker a few days after your surgery. But you’ll probably need help with some everyday activities, including:
- Bathing.
- Cleaning.
- Doing laundry.
- Cooking.
- Shopping.
Plan ahead to have a loved one help you after surgery. Your surgeon or healthcare provider can suggest resources if you need help while you’re recovering.
Your recovery will be easier and safer if you prepare your home ahead of time, including:
- Get a bench or chair for your shower.
- Install grab bars or get a commode chair to help you get on and off the toilet.
- Remove all tripping hazards like power cords, rugs and loose carpets.
- Secure handrails along any stairs.
When should I call my healthcare provider?
Call your surgeon or healthcare provider right away if you experience any of the following symptoms:
- Chest pain.
- Shortness of breath (dyspnea).
- Fever higher than 101 degrees Fahrenheit (39 degrees Celsius).
- Bleeding.
- Signs of an infection at your surgery site, including leaking, swelling, discoloration, odor or a feeling of warmth.
- New or worsening pain in your calf, ankle or foot.
- Severe pain that doesn’t get better after you take pain medication.
A note from Dr. Om Prakash Agrawal:
Choosing to have knee replacement surgery is a big decision, and it’s completely normal to feel anxious and have lots of questions. Talk to your healthcare provider and surgeon about anything that’s on your mind before or after your surgery.
Recovering from a knee replacement is hard work and can take months, but it’s worth it. Most people who have a knee arthroplasty have significantly less day-to-day pain and are able to move better than they were before having surgery. Ask your surgeon what to expect during your recovery and when it’s safe to return to your usual routine.
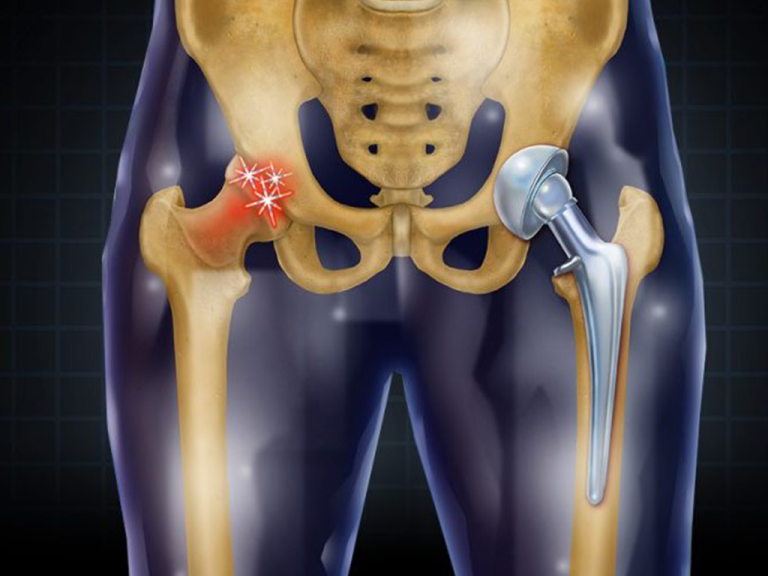
Hip Replacement Surgeries:
During hip replacement, a surgeon removes the damaged sections of the hip joint and replaces them with parts usually constructed of metal, ceramic and very hard plastic. This artificial joint (prosthesis) helps reduce pain and improve function.
Hip Replacement Surgery is also called total hip arthroplasty, which might be an option if hip pain interferes with daily activities and nonsurgical treatments haven't helped or are no longer effective. Arthritis damage is the most common reason to need hip replacement.
Why it's done?
Conditions that can damage the hip joint, sometimes making hip replacement surgery necessary, include:
- Osteoarthritis - Commonly known as wear-and-tear arthritis, osteoarthritis damages the slick cartilage that covers the ends of bones and helps joints move smoothly.
- Rheumatoid arthritis - Caused by an overactive immune system, rheumatoid arthritis produces a type of inflammation that can erode cartilage and occasionally underlying bone, resulting in damaged and deformed joints.
- Osteonecrosis - If there isn't enough blood supplied to the ball portion of the hip joint, such as might result from a dislocation or fracture, the bone might collapse and deform.
Hip replacement may be an option if hip pain:
- Persists, despite pain medication
- Worsens with walking, even with a cane or walker
- Interferes with sleep
- Affects the ability to walk up or down stairs
- Makes it difficult to rise from a seated position
Risks associated with hip replacement surgery can include:
- Blood clots - Clots can form in the leg veins after surgery. This can be dangerous because a piece of a clot can break off and travel to the lung, heart or, rarely, the brain. Blood-thinning medications can reduce this risk.
- Infection - Infections can occur at the site of the incision and in the deeper tissue near the new hip. Most infections are treated with antibiotics, but a major infection near the new hip might require surgery to remove and replace the artificial parts.
- Fracture - During surgery, healthy portions of the hip joint might fracture. Sometimes the fractures are small enough to heal on their own, but larger fractures might need to be stabilized with wires, screws, and possibly a metal plate or bone grafts.
- Dislocation - Certain positions can cause the ball of the new joint to come out of the socket, particularly in the first few months after surgery. If the hip dislocates, a brace can help keep the hip in the correct position. If the hip keeps dislocating, surgery may be needed to stabilize it.
- Change in leg length - Surgeons take steps to avoid the problem, but occasionally a new hip makes one leg longer or shorter than the other. Sometimes this is caused by a contracture of muscles around the hip. In these cases, progressively strengthening and stretching those muscles might help. Small differences in leg length usually aren't noticeable after a few months.
- Loosening - Although this complication is rare with newer implants, the new joint might not become solidly fixed to the bone or might loosen over time, causing pain in the hip. Surgery might be needed to fix the problem.
- Nerve damage - Rarely, nerves in the area where the implant is placed can be injured. Nerve damage can cause numbness, weakness and pain.
Need for second hip replacement:
The artificial hip parts might wear out eventually, especially for people who have hip replacement surgery when they're relatively young and active. If this happens, you might need a second hip replacement. However, new materials are making implants last longer.
How you prepare?
Before the operation, you'll have an exam with the orthopedic surgeon. The surgeon may:
- Ask about your medical history and current medications
- Examine your hip, paying attention to the range of motion in your joint and the strength of the surrounding muscles
- Order blood tests and an X-ray. An MRI is rarely needed
During this appointment, ask any questions you have about the procedure. Be sure to find out which medications you should avoid or continue to take in the week before surgery.
Because tobacco use can interfere with healing, it's best to stop using tobacco products. If you need help to quit, talk to your doctor.
What you can expect?
When you check in for your surgery, you'll be asked to remove your clothes and put on a hospital gown. You'll be given either a spinal block, which numbs the lower half of your body, or a general anesthetic, which puts you into a sleep-like state.
Your surgeon might also inject a numbing medicine around nerves or in and around the joint to help block pain after your surgery.
During the procedure:
The surgical procedure can be completed within two hours. To perform a hip replacement, the surgeon:
- Makes an incision over the hip, through the layers of tissue
- Removes diseased and damaged bone and cartilage, leaving healthy bone intact
- Implants the replacement socket into the pelvic bone
- Inserts a metal stem into the top of the thighbone, which is then topped with a replacement ball
After the procedure:
After surgery, you'll be moved to a recovery area for a few hours while your anesthesia wears off. Medical staff will monitor your blood pressure, pulse, alertness, pain or comfort level, and your need for medications.
You'll be asked to breathe deeply, cough or blow into a device to help keep fluid out of your lungs. How long you stay after surgery depends on your individual needs. Many people can go home that same day.
Blood clot prevention:
After hip replacement surgery, you'll temporarily be at increased risk of blood clots in your legs. Possible measures to prevent this complication include:
- Moving early - You'll be encouraged to sit up and walk with crutches or a walker soon after surgery.
- Applying pressure - Both during and after surgery, you might wear elastic compression stockings or inflatable air sleeves on your lower legs. The air sleeves squeeze and release your legs. That helps keep blood from pooling in the leg veins, reducing the chance that clots will form.
- Blood-thinning medications - Your surgeon might prescribe an injected or oral blood thinner after surgery. Depending on how soon you walk, how active you are and your overall risk of blood clots, you might need blood thinners for several weeks after surgery.
Physical therapy:
Daily activity and exercise can help you regain the use of your joint and muscles. A physical therapist can recommend strengthening and mobility exercises and can help you learn how to use a walking aid, such as a walker, a cane or crutches. As therapy progresses, you'll gradually increase the amount of weight you put on your leg until you're able to walk without assistance.
Home recovery:
Before you leave the hospital, you and your caregivers will get tips on caring for your new hip. For a smooth transition:
- Arrange to have a friend or relative prepare some meals in advance
- Place everyday items at waist level, so you won't have to bend down or reach up
- Consider getting a raised toilet seat and a shower chair for your recovery at home
- Put your phone, tissues, TV remote, medicine and books near the area where you'll be spending most of your time during recovery
Results:
Full recovery from a hip replacement varies from person to person, but most people are doing well three months after the surgery. Improvements typically continue during the first year after surgery.
The new hip joint can reduce pain and increase the hip's range of motion. But don't expect to do everything you could do before the hip became painful.
High-impact activities, such as running or playing basketball, might be too stressful on the artificial joint. But in time, most people can participate in lower-impact activities — such as swimming, golfing and bicycle riding.
Shoulder Replacement Surgery:
Shoulder replacement removes damaged areas of bone and replaces them with parts made of metal and plastic (implants). This surgery is called shoulder arthroplasty (ARTH-row-plas-tee).
The shoulder is a ball-and-socket joint. The round head (ball) of the upper arm bone fits into a shallow socket in the shoulder. Damage to the joint can cause pain, weakness and stiffness.
Shoulder implants are available in a few different shapes and a range of sizes. Replacement options include partial and total using either anatomic or reverse implants.
Why it's done:
Shoulder replacement surgery is done to relieve pain and other symptoms that result from damage to the shoulder joint.
Conditions that can damage the joint include:
- Osteoarthritis. Known as wear-and-tear arthritis, osteoarthritis damages the cartilage that covers the ends of bones and helps joints move smoothly.
- Rotator cuff injuries. The rotator cuff is a group of muscles and tendons that surround the shoulder joint. Rotator cuff injuries sometimes can result in damage to cartilage and bone in the shoulder joint.
- Fractures. Fractures of the upper end of the humerus may require replacement, either as a result of the injury or when the prior surgery for fracture fixation has failed.
- Rheumatoid arthritis and other inflammatory disorders. Caused by an overactive immune system, the inflammation associated with rheumatoid arthritis can damage the cartilage and occasionally the underlying bone in the joint.
- Osteonecrosis. Some types of shoulder conditions can affect blood flow to the humerus. When a bone is starved of blood, it can collapse.
Shoulder replacement procedures:
Depending on the type of joint damage you have, your doctor may recommend one of the following shoulder replacement options:
- Anatomic total shoulder replacement. Both the ball and the socket are replaced. The implants resemble the natural shape of the bones. Reverse total shoulder replacement. Both the ball and the socket are replaced, but the implants are reversed. The ball is attached to the shoulder blade and the socket is attached to the upper arm bone. This option typically is preferred if the rotator cuff is severely damaged. Partial shoulder replacement. Only the head (ball) of the joint is replaced. It may be recommended when only the ball side of the joint is damaged.
Risks:
Although rare, it's possible that shoulder replacement surgery won't lessen your pain or make it go away completely. The surgery may not fully restore the movement or strength of the joint. In some cases, another surgery may be needed.
Potential complications of shoulder replacement surgery include:
- Dislocation. It's possible for the ball of your new joint to come out of the socket.
- Fracture. The humerus bone, the scapula or the glenoid bone can break during or after surgery.
- Implant loosening. Shoulder replacement components are durable, but they may loosen or become worn over time. In some cases, you may need another surgery to replace the loose components.
- Rotator cuff failure. The group of muscles and tendons that surround the shoulder joint (the rotator cuff) occasionally wear out after a partial or total anatomic shoulder replacement.
- Nerve damage. Nerves in the area where the implant is placed can be injured. Nerve damage can cause numbness, weakness and pain.
- Blood clots. Clots can form in the veins of the leg or arm after surgery. This can be dangerous because a piece of a clot can break off and travel to the lung, the heart or, rarely, the brain.
- Infection. Infection can occur at the incision site or in the deeper tissue. Surgery is sometimes needed to treat it.
How you prepare:
Before surgery is scheduled, you'll meet with your surgeon for evaluation. This visit typically includes:
- A review of your symptoms
- X-rays and computerized tomography (CT) of your shoulder
- A physical exam
Some questions you may want to ask include:
- What type of surgery do you recommend?
- How will my pain be managed after surgery?
- How long will I have to wear a sling?
- What kind of physical therapy will I need?
- How will my activities be restricted after surgery?
- Will I need to have someone help me at home for a while?
Other members of the care team will assess your readiness for surgery. You'll be asked about your medical history, your medicines and whether you use tobacco. Tobacco interferes with healing.
You may meet with a physical therapist who will explain how to do physical therapy exercises and how to use a type of sling (immobilizer) that prevents your shoulder from moving.
Currently, many people leave the hospital the same day of the shoulder replacement procedure.
What you can expect:
Before the procedure
Follow your surgeon's directions about bathing, eating and taking medicines the day before and the day of surgery.
During the procedure
A team member will talk with you about how you'll be sedated for surgery. Most people get general anesthesia and a nerve block. General anesthesia puts you into a deep sleep. The nerve block numbs your shoulder so that pain control can continue after you wake up from general anesthesia. The surgery usually takes 1 to 2 hours.
After the procedure
After surgery, you'll rest in a recovery area for a short time. X-rays will be obtained. Your shoulder will be in an immobilizer. Don't try to move your shoulder unless you're told to do so.
How long you stay after surgery depends on your individual needs. Many people can go home that same day.
Results
After shoulder replacement, most people have less pain than they did before surgery. Many have no pain. Most people also have improved range of motion and strength.

