
Knee arthroscopy:
Knee arthroscopy is a minimally invasive surgical procedure. Healthcare providers use knee arthroscopy to diagnose and treat a range of knee injuries. Your healthcare provider makes a small incision and then inserts a long, thin tool with a camera on the end. The camera shows images of the inside of your knee, which helps your healthcare provider make a diagnosis of your injury.
What is knee arthroscopy?
Healthcare providers use knee arthroscopy to diagnose and treat a wide range of knee injuries. During arthroscopic knee surgery, your healthcare provider inserts a tiny camera through an incision. The camera shows the inside of your knee. The images appear on a screen in the operating room. They help your healthcare provider diagnose problems inside of your knee. Knee arthroscopy is a very common minimally invasive surgical procedure. Minimally invasive procedures require smaller incisions (cuts) than traditional surgery.
The incisions are about the size of a keyhole. To treat injuries or structural problems, your healthcare provider inserts tiny tools through another incision. They use the tools to repair or remove damaged tissue.
Who needs knee arthroscopy?
Your healthcare provider may recommend knee arthroscopy if you have knee pain that doesn’t get better with nonsurgical treatments. Nonsurgical treatments include rest, ice, nonsteroidal anti-inflammatory drugs and physical therapy (PT). Although arthritis causes knee pain, arthroscopic knee surgery isn’t always an effective treatment for osteoarthritis.
Healthcare providers use arthroscopy to get a better look at cartilage, bones and soft tissues inside of your knee. They use the procedure to diagnose several types of knee injuries. Most of these injuries affect ligaments and cartilage in your knee joint.
Knee injuries among athletes (including adolescents) are very common. They can happen in contact sports and those that require jumping, such as volleyball.
Why do providers use knee arthroscopy?
Your healthcare provider uses knee arthroscopy to:
- Diagnose injuries: During knee arthroscopy, your healthcare provider takes a close look at any painful or swollen areas. The camera shows images of damaged soft tissues and bones. The images help your healthcare provider diagnose injuries (or confirm a diagnosis) and plan treatment.
- Repair injured soft tissues and bones: If you need surgery to repair tendons, ligaments or cartilage, your healthcare provider uses specially designed tools. The camera shows real-time images that guide your healthcare provider during the procedure. Your healthcare provider uses tiny tools to repair and reconstruct soft tissues by stitching them together. They can also suture (stitch) bones together.
- Remove damaged or inflamed tissue: Some tiny tools help your healthcare provider shave off damaged bone and cartilage or inflamed tissue (such as the synovium). They use tools to remove these tissues from your knee.
What conditions does knee arthroscopy treat?
You may need knee arthroscopy if you have:
- Soft tissue injuries: Soft tissues include ligaments (they connect bones to bones) and tendons (they connect muscles to bones). Some of the most common knee injuries are bursitis, torn meniscus, patellar tendonitis, anterior cruciate ligament tear (ACL tear) and tears of the medial collateral ligament (MCL tear).
- Fracture: Bones can break or chip off inside of your knee. Sometimes, pieces of cartilage (rubbery tissue that helps bones move against each other smoothly) can break off when your bone fractures.
- Inflammation: The synovium inside a joint can become inflamed (swollen and irritated). Synovium is soft tissue on the inside of a joint. Healthcare providers call this condition synovitis.
Procedure Details
What happens before knee arthroscopy?
Before you have knee arthroscopy, tell your healthcare provider what medications you’re taking. You may need to stop taking certain medications (such as blood thinners) before surgery. Your healthcare provider will tell you what time to stop eating and drinking the night before your procedure, too.
You may have knee arthroscopy at a surgery clinic or in a hospital. Right before your procedure, your healthcare provider will give you anesthesia. Whether you’re awake or asleep, you won’t feel pain during knee surgery. Your healthcare provider may recommend:
- Local anesthetic, to numb the area.
- Regional anesthetic, to numb you from the waist down.
- General anesthetic, to put you to sleep for the procedure.
What happens during knee arthroscopy?
During the procedure, your healthcare provider:
- Cleans your leg and secures your knee in a stabilizing device. The device ensures that your knee stays in the proper position throughout the procedure.
- Makes a small incision (cut) in your knee and inserts a long metal tool called an arthroscope into the incision. The arthroscope has a camera on the end. Images from the camera appear on a screen in the operating room.
- Looks at the images on the monitor and uses them to diagnose injuries and guide the procedure. If you need surgery, your healthcare provider makes other incisions in your knee and inserts tiny tools through them.
- Repairs torn tissues, shaves off damaged bone or cartilage and removes inflamed or damaged tissues. Your healthcare provider uses specially designed tools for these tasks.
- Closes the incisions with stitches or small bandages, and wraps your knee with a larger bandage or dressing.
What happens after knee arthroscopy?
Most knee arthroscopies are outpatient procedures, meaning you go home the same day. They usually take about an hour. Sometimes, knee arthroscopy requires a hospital stay (inpatient procedure).
When you’re ready to go home, you’ll need someone to drive you. After surgery, you’ll feel some pain. While recovering the first few days after your procedure, you should:
- Stay off of your feet: Avoid putting weight on your knee for a few days. You may need crutches or a walker to help you get around.
- Elevate your knee: To reduce swelling and relieve pain, rest with your leg elevated. Try to keep your knee above your heart.
- Take pain medication: Your healthcare provider may recommend over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) or prescription pain medication. Be sure to follow your healthcare provider’s instructions when taking pain medication. You may also need drugs to reduce swelling or prevent blood clots.
- Keep your incisions covered. Make sure the bandage stays on your knee, and keep the area clean. Ask your healthcare provider when you can remove the dressing, take a shower or bathe after your procedure.
After you’ve had time to heal from the procedure, your healthcare provider may recommend physical therapy (PT). A customized PT program can help you gain strength and mobility. Your physical therapist will show you special exercises to increase flexibility, strengthen the muscles that support your knee and avoid another injury.
Risks vs Benefits:
What are the advantages of knee arthroscopy?
Minimally invasive procedures like knee arthroscopy usually require less recovery time than traditional (open) surgery. As you only need a few small stitches, you’re more likely to get back on your feet more quickly than with traditional surgery. You may also have less pain and a lower risk of infection.
What are the risks or complications of knee arthroscopy?
Complications from knee arthroscopy are rare. As with any surgery, risks of knee arthroscopy include bleeding and infection.
After the procedure, some people have:
- Blood clots.
- Knee stiffness.
- Swelling that results from blood pooling in the knee (this complication is uncommon).
When can I go back to my usual activities after knee arthroscopy?
Everyone responds to surgery differently. Ask your healthcare provider when you can get back to your daily activities, including driving and walking without assistance. Your healthcare provider may recommend waiting several weeks before doing more physical or strenuous activities.
Sometimes, people need to make changes to their lifestyle and activity level. Some sports (especially those that require running or jumping) can damage your knee. Talk to your healthcare provider about choosing lower-impact sports and activities that are easier on your knee.
When should I see my healthcare provider about knee arthroscopy?
Call your healthcare provider if you have:
- Bleeding.
- Signs of infection, including fever, severe swelling or drainage (pus) from the incisions.
- Pain that’s severe or doesn’t go away with pain relief medications.
A note from Dr. Om Prakash Agrawal:
Knee arthroscopy procedures are safe and effective. They help healthcare providers diagnose and treat a wide range of injuries without the need for large incisions. Minimally invasive techniques usually require less recovery time than traditional (open) surgery. If your healthcare provider recommends a PT program after the procedure, follow instructions carefully. Sticking to a PT program can help you get back on your feet after surgery.
Shoulder arthroscopy:
Shoulder arthroscopy is a type of surgery used to diagnose and treat shoulder problems. Your healthcare provider repairs your shoulder through tiny incisions. Shoulder arthroscopy is an outpatient procedure, meaning you can go home the same day. Though full recovery can take weeks or months, exercise and physical therapy can help with healing.
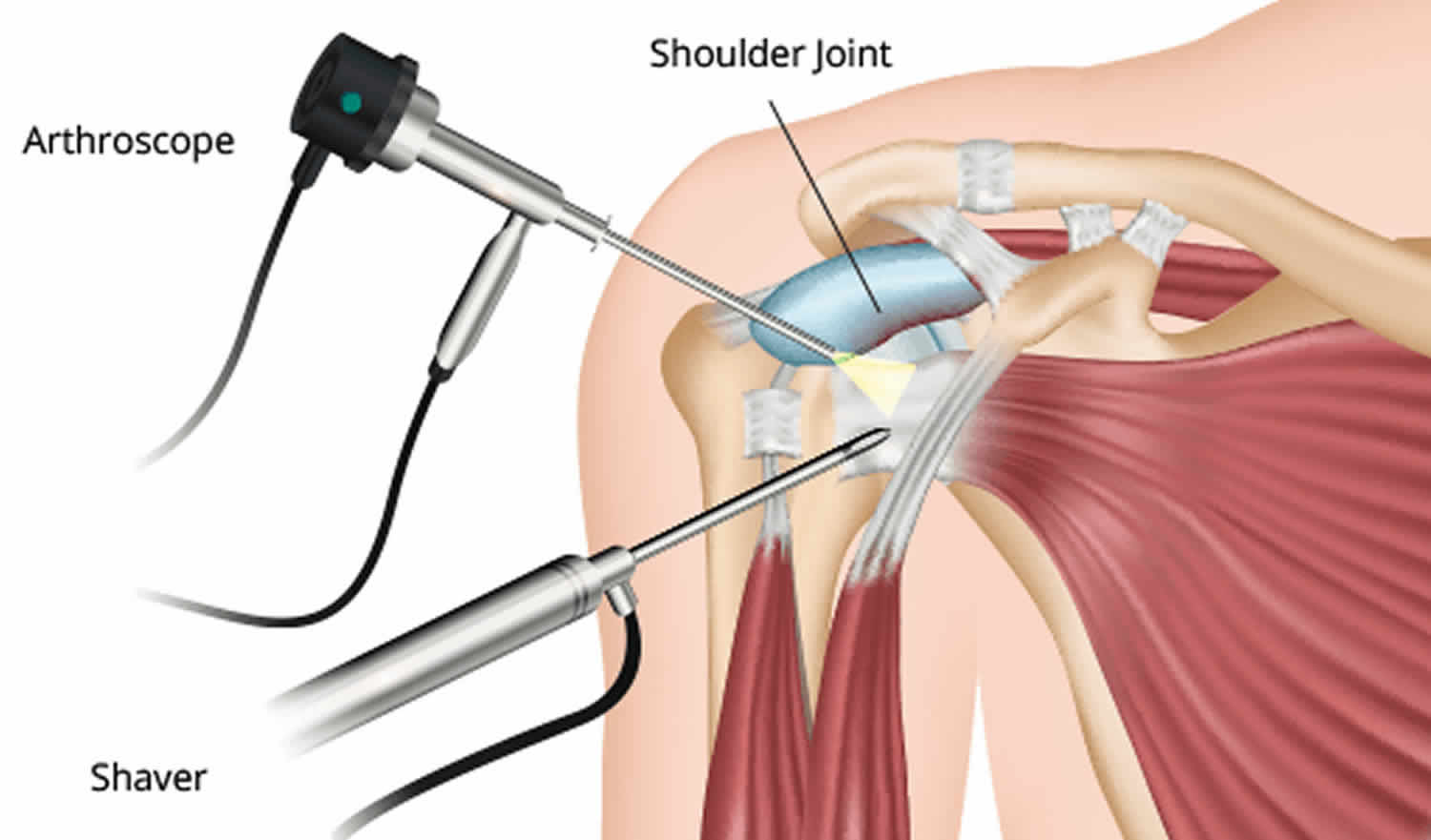
What is shoulder arthroscopy?
Shoulder arthroscopy is a minimally invasive surgery used to diagnose and treat shoulder problems. You might have arthroscopy for rotator cuff tears or shoulder impingement. Minimally invasive procedures require smaller incisions than traditional surgery. Each incision is about the size of a keyhole.
Your surgeon inserts a small camera called an arthroscope through a tiny incision in your skin. This camera projects pictures of your shoulder joint to a video screen. Your provider looks at these images to find the source of your injury. If you need a shoulder repair, the provider uses miniature surgical instruments to restore your shoulder’s mobility.
Why is shoulder arthroscopy done?
Shoulder arthroscopy helps healthcare providers find and treat shoulder pain that has not responded to nonsurgical treatments. Nonsurgical treatments for shoulder pain include physical therapy, medication, injections and rest.
What shoulder injuries does arthroscopic shoulder surgery treat?
Shoulder arthroscopy can remove inflamed tissue. It can also treat injuries such as:
- Biceps tendon injuries.
- Bone spurs.
- Frozen shoulder.
- Labrum tears, injuries to the tissue around your shoulder socket.
- Osteoarthritis.
- Rotator cuff tears.
- Rotator cuff tendinitis.
- Shoulder impingement syndrome.
- Shoulder instability, when your shoulder joint becomes loose or dislocated.
How common is shoulder arthroscopy?
Shoulder arthroscopy is the second most common orthopedic surgery after knee arthroscopy. Orthopedic surgery treats joints, bones, muscles, ligaments and tendons. Rotator cuff surgery is one of the most common types of shoulder arthroscopy.
What happens before arthroscopic shoulder surgery?
Before shoulder arthroscopy, your provider will ask you about your health history. You’ll also need to bring in a complete medication list. You may need to stop taking some of your medications a few days before your surgery.
Your hospital will give you specific instructions, including how long before your surgery to stop eating and drinking.
To check your health before your procedure, you also may need:
- Blood tests.
- A chest X-ray.
- Electrocardiogram.
What happens during shoulder arthroscopy?
Shoulder arthroscopy usually takes less than an hour. During shoulder arthroscopy:
- You will be in a semi-seated position (beach chair position) or lying on your side.
- Your surgical team will shave hair (if needed) and clean your skin with an antiseptic solution. They may place your arm in a holding device to make sure it stays still.
- A healthcare provider may inject fluid into your shoulder. The fluid inflates your shoulder joint, making it easier for the surgeon to see.
- Your surgeon makes a small hole, usually about the size of a buttonhole, in your shoulder. They insert the tiny camera (arthroscope) into this incision.
- The camera projects images of your shoulder to a video screen. Your surgeon uses these images to find the problem with your shoulder.
- Your surgeon makes other small cuts in your shoulder and inserts tiny instruments.
- Once your surgical team finishes your surgery, they close the incisions. You may have stitches or small bandages, with a large bandage on top.
What happens after shoulder arthroscopy?
Shoulder arthroscopy is an outpatient procedure, meaning you can go home the same day. The entire process usually takes less than an hour.
You’ll need to recover for an hour or two at the hospital after surgery. Your providers will offer pain medication if needed. After that, you’ll need a ride home. It’s best if a family member or friend can spend the night with you.
How painful is shoulder surgery?
Unfortunately, all surgery causes pain. But your hospital’s anesthesia staff focus on keeping you comfortable during surgery. They will discuss options with you.
During surgery, shoulder arthroscopy often uses nerve blocks injected into your neck or shoulder. These nerve blocks numb your shoulder and arm. They also help with pain relief after surgery. In some cases, you may have general anesthesia, where you are asleep during your surgery.
Pain during recovery is a natural part of healing. Talk with your healthcare providers about your concerns. They can advise you on how to manage pain as your body heals.
Risks vs Benefits:
What are the advantages of arthroscopic shoulder surgery?
You may have shoulder arthroscopy instead of open surgery (with a larger incision), depending on your specific concern. Compared to open surgeries, arthroscopic surgeries have less risk of infection and a shorter recovery time. Shoulder arthroscopy also tends to cause less joint stiffness and pain than open surgeries.
What are the risks or complications of shoulder arthroscopy?
Shoulder arthroscopy is generally very safe. There is a small risk that you may experience:
- Blood clots.
- Damage to blood vessels or nerves.
- Excessive bleeding or swelling.
- Infection.
What is the recovery time after shoulder surgery?
- Your shoulder joint will take weeks to months to completely heal after shoulder arthroscopy. You may notice pain and swelling for at least several weeks.
- Ice and pain medication can help with pain relief. You can also try sleeping propped up in a chair or bed for a few days after your surgery. Your surgeon may recommend a sling to protect your shoulder.
- A rehabilitation plan includes gentle exercise and physical therapy. It can increase your shoulder movement and strength. Your healthcare provider will give you a rehab plan that suits your specific shoulder surgery.
When can I go back to work/school/drive/eat?
When you can return to your everyday life depends on the complexity of your surgery. If you’ve had a minor procedure, you may be able to return to work or school in a few days. You’ll need longer to recover from more major procedures. Your healthcare provider will offer guidance suitable for your recovery.
When To Call the Doctor or when should I see my healthcare provider?
Talk to your healthcare provider if you have any of these symptoms after your surgery:
- Fever.
- Pain that medication doesn’t help.
- Discolored or smelly fluid around the wound.
- Tingling or numbness.
- Increased swelling.
A note from Dr. Om Prakash Agrawal :
Shoulder arthroscopy is a minimally invasive surgery to treat shoulder problems, including shoulder impingement and rotator cuff tears. The procedure usually takes less than an hour. Many people can go back to work or school in a few days. For more complex surgeries, recovery may take longer. A rehabilitation plan, which usually includes exercise and physical therapy, can help you heal faster.
Sports injuries:
The term “sports injury” refers to the kinds of injuries that most commonly occur during sports or exercise, but they are not limited to athletes. Factory workers get tennis elbow, painters get shoulder injuries, and gardeners develop tendinitis, even though they may not participate in sports. Ultimately, however, “sports injuries” refers to those that occur in active individuals. This health topic focuses on the most common types of sports injuries—those that affect the musculoskeletal system. The musculoskeletal system is the network of muscles, tendons, ligaments, bones, and other tissues that provides the body with stability and enables movement.
Sports injuries are divided into two broad categories, acute and chronic injuries. Acute injuries happen suddenly, such as when a person falls, receives a blow, or twists a joint, while chronic injuries usually result from overuse of one area of the body and develop gradually over time. Examples of acute injuries are sprains and dislocations, while some common chronic injuries are shin splints and stress fractures.
Treatment for a sports injury depends on the type of injury, but minor ones can usually be treated at home by resting, icing, compressing, and elevating (R-I-C-E) the injured part of the body. For more serious injuries, you will need to see a health care provider, and you may need to be set up for a course of physical therapy for rehabilitation and/or fitted for a cast, splint, or brace. In some cases, you may need surgery. A rehabilitation program that includes exercise and other types of therapy is usually recommended before resuming the sport or activity that caused the injury.
Who Gets Sports Injuries?
Anyone can suffer a sports injury, but several factors can increase the risk of sustaining injury.
The risk factors for sports injuries include:
- Not using the correct exercise techniques.
- Overtraining, either by training too often, too frequently, or for too long.
- Changing the intensity of physical activity too quickly.
- Playing the same sport year-round.
- Running or jumping on hard surfaces.
- Wearing shoes that do not have enough support.
- Not wearing the proper equipment.
- Having had a prior injury.
- Having certain anatomical features specific to each joint or poor flexibility.
- Taking certain medications, such as fluoroquinolones, a class of antibiotics linked to tendinitis and tendon rupture.
The type of injury you are most vulnerable to depends on the type of activity you participate in, your age, and your sex.
Types:
Sports injuries are broadly categorized into two kinds:
- Acute injuries, which happen suddenly.
- Chronic injuries, which are usually related to overuse and develop gradually over time.
In some cases, wear and tear from overuse injuries can set the stage for acute injuries.
Types of Musculoskeletal Injuries:
Injuries to the musculoskeletal system that are common in athletes include fractures, dislocations, sprains, strains, tendinitis, or bursitis. These terms are defined below.
- Bone fracture - A fracture is a break in a bone that occurs from either a quick, one-time injury, known as an acute fracture, or from repeated stress, known as a stress fracture. Growth plate fractures are unique to children who are still growing.
- Acute fractures. A fall, car accident, or blow can cause a fracture, and the severity depends on the force that caused the break. The bone may crack, break all the way through, or shatter. Injuries that break through the skin to the bone, which are known as compound fractures, are especially serious because there is an increased risk of infection. Most acute fractures are emergencies.
- Stress fractures. Stress fractures occur largely in the weight-bearing bones of the lower extremity. These include the femur, tibia and fibula, and foot bones. They are common in sports where there is repetitive impact, primarily running or jumping sports such as gymnastics, tennis, basketball, or track and field. Running creates forces two to three times a person’s body weight on the lower limbs.
- Growth plate fractures. The growth plate is an area of cartilage near the ends of long bones, and they enable the bones to lengthen until children reach their full height. Growth plates are especially vulnerable to injury until they are converted to bone, typically by the time a child reaches the age of 20. Growth plate fractures can result from a single traumatic event, such as a fall or car accident, or from chronic stress and overuse.
- Dislocation - When the two bones that come together to form a joint become separated, the joint is described as dislocated. Contact sports such as football and basketball, as well as high-impact sports and sports that involve significant stretching or falling, cause most dislocations. A dislocated joint typically requires immediate medical treatment, but sometimes the bones move back into place on their own. A dislocation is a painful injury and is most common in shoulders, elbows, fingers, kneecap, and femur-tibia or knee.
- Sprain - Sprains are stretches or tears of ligaments, the bands of connective tissue that join the end of one bone with another. Sprains are caused by trauma such as a fall or blow that knocks a joint out of position. Sprains can range from first degree (minimally stretched ligament) to third degree (a complete tear). Areas of the body most vulnerable to sprains are ankles, knees, and wrists.
- Strain - A strain is a twist, pull, or tear of a muscle or tendon, a cord of tissue connecting muscle to bone. Athletes who play contact sports can get strains, but they can also happen from repeating the same motion again and again, as in tennis or golf. Like sprains, strains can range from a minor stretch to a partial or complete tear of a muscle or tendon. This is most common in muscle or tendons between two joints.
- Tendinitis - Tendinitis is inflammation of a tendon, a flexible band of fibrous tissue that connects muscles to bones. It often affects the shoulder, elbow, wrist, hip, knee, or ankle. Tendinitis can be caused by a sudden injury, but it usually results from carrying out the same motion over and over. People such as carpenters, gardeners, musicians, and certain types of athletes, such as golfers and tennis players, have a higher risk of tendinitis. Tendons become less flexible as you age, so you are more likely to get tendinitis as you get older.
- Bursitis - Bursitis is inflammation of the bursae (plural of “bursa”), small, fluid-filled sacs that act as cushions between a bone and other moving parts, such as muscles, tendons, or skin. Bursitis can be caused by a one-time event like a blow or fall. It can also result from repeating the same motion many times, like throwing a ball, or from prolonged pressure, such as from kneeling on a hard surface or leaning on the elbows. It usually affects the shoulders, elbows, hips, or knees.
Common Sports Injuries:
Most sports injuries involve one or more of the types of musculoskeletal injuries described above. The joints are particularly susceptible because a person’s body places significant demands on them. Joints must provide both stability and flexibility, and they are complex structures that include several interconnected parts.
Some of the common injuries experienced by athletes and people who have jobs or hobbies that involve doing a repetitive motion include:
-
Shoulder Injuries:
- Rotator cuff injury - These are the most common shoulder injuries. The rotator cuff is a group of four muscles and tendons that stabilize the shoulder joint. Rotator cuff injuries happen when the tendons or bursae near the joint become inflamed from overuse or a sudden injury. They are common in people with jobs that involve overhead motions, like painters, or athletes who repeatedly reach upward, such as tennis players and swimmers.
- Impingement - This happens when the top of the shoulder blade puts pressure on the soft tissues beneath it when the arm is lifted. Tendinitis and bursitis can develop, limiting movement and causing pain. Repeated overhead movements, such as those used by swimmers, increase the risk of impingement.
- Instability - Shoulder instability happens when the round end of the upper arm bone is forced out of its shallow socket, either partially or completely. Once the tendons, ligaments, and muscles of the shoulder become stretched or torn, the shoulder becomes “loose” and dislocations can occur repeatedly.
-
Elbow Injuries
- Tennis elbow (lateral epicondylitis). When you play tennis or other racket sports, the tendons in the elbow can develop small tears and become inflamed, causing pain on the outside of the elbow. Painters, plumbers, carpenters, and others who repetitively use their forearms are also at higher risk of getting tennis elbow.
- Golfer’s elbow (medial epicondylitis). This is a form of tendinitis that causes pain in the inner part of the elbow. Pain may spread to the forearm and wrist. Golfers and others who repeatedly use their wrists or clench their fingers can develop it.
- Little league elbow. This is a growth plate injury to the elbow caused by repetitive throwing in youths. It is most common in pitchers, but any young athlete who throws repeatedly can get it. The pain is in the inner part of the elbow.
- Ulnar collateral ligament injury. Repeated throwing can cause tears to this ligament on the inner part of the elbow, causing pain and decreased throwing effectiveness.
Knee Injuries:
- Runner’s knee. Also called jumper’s knee or patellofemoral pain syndrome, this condition causes pain or tenderness close to or under the kneecap (patella) at the front of the knee. It is common in runners, but it also affects people who are active in other ways, such as those who hike or cycle.
- Fracture. Fractures can happen in any bone around the knee, but the kneecap (patella) is the most common, usually as a result of an event like a bad fall or a blow to the knee.
- Dislocation. A large impact to the knee can cause the kneecap to be forced from the groove in the thigh bone (femur) and pushed out of alignment, causing the kneecap to slip out of position.
- Torn ligament. When the knee is over-extended or twisted, the ligaments within it can tear. Anterior cruciate ligament (ACL) injuries are especially common in athletes. They often happen when the person changes direction suddenly or lands from a jump.
- Meniscal tear. Meniscal cartilage serves as a shock absorber in the knee. An awkward twist or pivot can cause a tear. They are commonly torn when the knee suffers a sprain or complete tear of the knee ligaments.
- Tendon tear. Tendon tears tend to be more common in middle-aged people who play sports that involve running and jumping. They often happen because of a forceful landing and sometimes from an awkward jump.
Leg Injuries:
- Groin pull. Quick side-to-side motions can strain the muscles of the inner thighs and lead to a groin pull. People who play sports such as hockey, soccer, football, and baseball have a higher risk of groin pulls.
- Hamstring strain. Three muscles run along the back of the thigh and form the hamstring. Activities that involve a lot of running, jumping, and sudden starts and stops place you at risk of a hamstring strain. Basketball, football, and soccer players commonly get them.
- Shin splints. Shin splints refers to the pain caused by inflammation of the muscles, tendons, and bone tissue along the inside length of the shinbone (tibia), the large bone in the front of the lower leg. The pain is usually on the inner side of the lower leg. Shin splints are primarily seen in runners, particularly those just starting a running program.
Ankle Injuries
- Ankle sprain. You can sprain your ankle when you roll, twist, or turn your ankle in an awkward way, stretching or tearing the ligaments in the joint. It can happen when you land awkwardly when jumping or pivoting, when walking on an uneven surface, or when someone else lands on your foot. People who play sports in which there is a lot of pivoting, such as volleyball and basketball, are at risk of an ankle sprain.
- Achilles tendinitis. An Achilles tendon injury results from a stretch, tear, or irritation to the tendon connecting the calf muscle to the back of the heel. The Achilles is the largest tendon in the body and you use it when you walk, run, climb stairs, jump, and stand on the tips of your toes. People with Achilles tendinitis usually feel pain and stiffness at the back of the heel, especially in the morning. Achilles tendinitis is usually a chronic condition caused by overuse, but serious cases can lead to a tear that may require surgery.
Symptoms of Sports Injuries:
The symptoms of a sports injury depend on the type of injury you have.
Symptoms of an acute injury include:
- Sudden, severe pain.
- Extreme swelling or bruising.
- Not being able to place weight on a leg, knee, ankle, or foot.
- Not being able to move a joint normally.
- Extreme weakness of an injured limb.
- A bone or joint that is visibly out of place.
Symptoms of a chronic injury due to overuse include:
- Pain when you play or exercise.
- Swelling and a dull ache when you rest.
Cause of Sports Injuries
The cause of an acute sports injury is a force of impact that is greater than the body part can withstand, while a chronic injury is typically due to repeating the same motion over and over again. Sometimes, overuse injuries can degrade tissues and joints and set the stage for an acute injury.

